Improving Population Health with Data Analytics
One client's journey to a modern, cloud-based data platform to support value-based care initiatives.

The Client
A Value-Based Care Consulting
& Population Health Analytics Services Company
The Business Objective
Our client’s core business focused on enabling healthcare providers to maximize incentives received from payer value-based programs, while also improving quality of care and optimizing operations. As value-based care expanded across the industry, our client wished to broaden their market reach and increase service offerings.
Foundational to the success of this growth was developing a new way for client analysts and data scientists to help physician partners quickly identify quality improvement and gaps in care closure opportunities, while also taking a deeper look into revenue generating and cost savings options. However, the client’s current vendor solution was complicated, slow, manual, and inhibited their ability to derive actionable insights to bring about improvements.
The Business Impact
- 50%
Improvement in quality performance for 900 network physicians
- 2M+
Patient gaps in care closed
- 11.5%
Medical spend reduction for ACO client
Recommended Content
Simply collecting data is not enough. Healthcare organizations must unlock actionable insights they can apply across the enterprise to improve patient care, ensure compliance, personalize customer experiences and accelerate innovation.
The Solution
A modern cloud-based data platform for supporting all value-based and provider analytics and reporting.
Data Integration
Plan (member, claims, provider, gaps, and risk data), Clinical, and HIE
- 8 Health Plans
- 12+ EMRs
- 100+ Clinics
- 4 HIEs
Reporting & Analytics
- Provider Quality – HEDIS (30 measures), EBCR and analytics, gaps in care and treatment opportunities, cost and utilization trends
- PCMH and Physician Incentive Programs
- Revenue Management
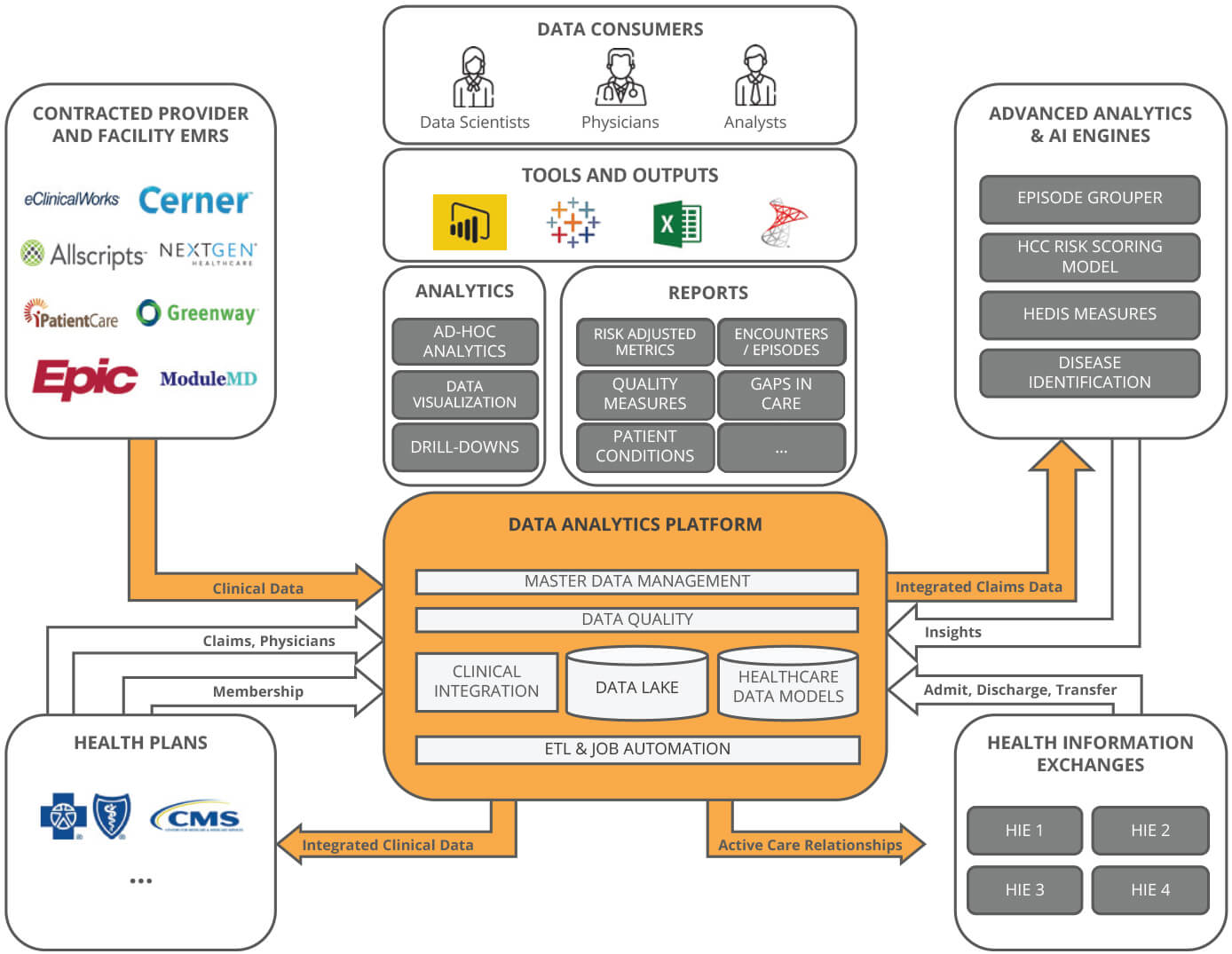
X by 2 Accelerator Solutions Leveraged
- Clinical Data Integration Solution
Adapts to EMR vendors across hundreds of healthcare providers, quickly addressing data variations and customizations and shortening time to insight.
- Data Quality Solution
Fit-for-purpose solution enabled our client to rapidly target and remediate their most critical data quality issues. Data health dashboard provides real-time data quality checks and dynamic data management.
- Healthcare Data Models
Proven models reduced time to value through integration of data into enterprise reporting, analytics and operational processes, increasing interoperability and improving outcomes.
- Use Cases
Bringing all of the data together in order to identify gaps in care and treatment opportunities, disease and chronic disease identification, as well as cost and utilization trends.
The Results
The X by 2 approach improved and modernized key areas:
Architecture
- Before: Rigid
Lack of external integration points and data accessibility
- After: Flexible
Scalable, cloud-based platform able to grow with increased demands
Processes
- Before: Vendor Dependent
Cumbersome workflows, manual processes still required
- After: Self-Sufficient
Automated workflows, self-service reporting, data gathering
Software/Tools
- Before: Heavy
Complex and slow to change with expensive/recurring vendor costs
- After: Lightweight
Easier onboarding and training; increased speed to market
Data/Reports
- Before: Fragmented
Data across repositories, lack of canned reports, poor data quality
- After: Consolidated
Reduced complexity, automated reporting, improved data quality