Claims System Modernization
How one client reimagined user experience to develop an innovative, agile claims modernization strategy.
The Client
Health Insurance Core System &
Digital Solution Provider
The Business Objective
Our client provides core system and digital health solutions for leading health plans. X by 2 created a strategy and roadmap for the client’s core product offerings followed by a targeted analysis of their mainframe claims processing system. The goal? To turn the claims system, which processes approximately 288 million claims per year, auto-adjudicates 90% of all claims and supports nearly 20 million members, into an industry-leading commercial claims processing platform.
The client’s system was fast, efficient, and accurate, but its legacy technology made attracting and onboarding new users difficult. In order to meet user demands in a changing workforce and navigate increasingly complex claims orchestration processes, our client needed:
- A modernized user experience
- Improved usability, efficiency, and productivity through a greater level of process transparency, workflow automation, and AI-driven insight
- Increased agility and adaptability
The Business Impact
- Immediate UX Improvements
Address user pain points while the legacy system is replaced over time.
- Contextualized Claims
Make research and complex adjustments more productive for claims representatives.
- Reduced Development & Support Costs
Increase system flexibility to enable agile development of updates and new features.
- New Client Acquisition & Improved Retention
Meet changing customer needs with faster onboarding, reduced friction, and ease of use.
The Business Outcome
With a phased, agile development approach, X by 2 introduced a top-down claims modernization strategy and roadmap to help the client reimagine their legacy system.
Recommended Content
The Project Challenges
During the discovery phase we faced:
- A vast, 4000+ mainframe screen system, making data collection a challenge.
- An accelerated timeline to modernize the UX without impacting the critical claims system.
- The need for an adaptable interface, capable of meeting various business requirements.
The Project Approach
Leveraging our unique, combined expertise in UX and software architecture, we envisioned:
- A focused technology strategy involving a robust API gateway to simplify data access and enable AI capabilities.
- A user-friendly interface built on top of the legacy claims system, making data collection more accessible on the front end.
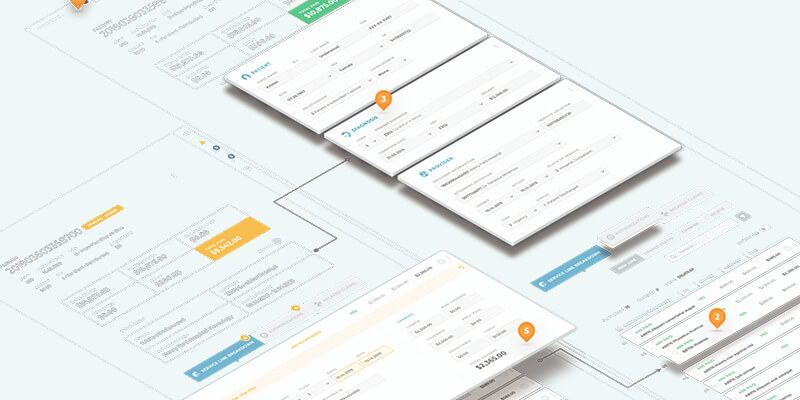
- A centralized workspace with flexible interface templates and customizable content comparison capabilities.

The Work
UX Research & Vision
- Developed user personas and mapped user needs to core experiences and journeys
- Constructed an integrated, user-centric experience around business, process, and technology needs
- Developed a comprehensive set of solution requisites
- Explored and visualized UX/UI concepts
- Conducted UX-based vendor assessment and selection
Technology Strategy
- Developed logical and technical future state architectures
- Identified opportunities to leverage AI models for claims auto-assignment; OON negotiation; and fraud, waste, and abuse reduction
- Evaluated technology and vendor options; conducted vendor technical review
- Established solution vision, technical architecture, and transition strategy to support the client’s core services, features, and functionality
Transformation Roadmap
- Conceptualized a modern, user-centric experience and reimagined claims workbench and workflows
- Recommended technical architecture, tools, and technology
- Developed UX/UI and legacy “core engine” modernization strategy
- Prioritized and aligned roadmap and execution plan with business goals
- Created team structure, timeline, and cost estimation
Proof of Concept
- UX/UI clickable prototype
- Proof of concept for key business use cases and workflows to prove out capabilities
